As a follow-up to the discussions we have had about too-high cesarean rates, we are talking about late complications from cesareans, especially in future pregnancies after a cesarean.
In particular, the risk for abnormal placentation rises with each successive cesarean. These include:
- placental abruption (the placenta shearing off before the baby is ready to be born)
- placenta previa (a low-lying placenta that covers or nearly covers the cervix)
- placenta accreta (an abnormally attached placenta that has difficulty detaching after birth)
Types of Placenta Accreta
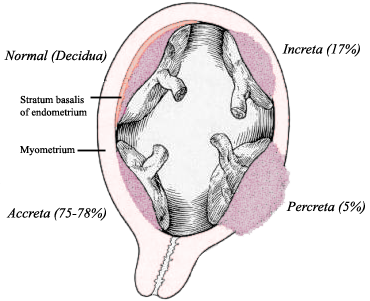
As mentioned in Part One of this series, placenta accreta is an abnormally attached placenta. However, the severity can vary, leading to three different types of "morbidly adherent" placentas.
To review, each month the lining of a woman's uterus (the endometrium) changes in anticipation of a possible pregnancy, becoming the decidua if pregnancy occurs. Among other functions, the decidua helps keep the placenta from invading the mother's uterus.
In placenta accreta, the decidua is thin or deficient, allowing the placenta to attach itself directly into the maternal tissues. How deeply it attaches determines the severity of the accreta.
In an accreta, the placenta invades the deficient decidual layer and attaches to the wall of the uterus. About 75% of accretas are in this form, where the placenta is morbidly adherent to the the uterus but has not grown deeply into it. Some cases are relatively minor, while others are quite serious, depending on how much and how strongly the placenta is abnormally attached.
In Placenta Increta, the placenta actually grows deeply into the muscle of the uterus (myometrium). It is nearly impossible for these placentas to detach unless they are cut out. This can lead to massive hemorrhages that often necessitate a hysterectomy. It is a very serious complication.
In the most severe form, Placenta Percreta, the placenta grows not only into the muscle of the uterus but through the outer layer (serosa) and often into adjacent structures nearby. This is an extremely life-threatening complication because percretas usually grow into the mother's bladder or bowels, the uterus may rupture, and women can suffer severe injuries or even die from it.
Thankfully, most accretas don't involve an increta or a percreta. But even on its own, accreta is a serious complication.
Fortunately, foreknowledge of an accreta, careful management protocols, and being in the right delivery setting can significantly lower the risk for mortality and morbidity. But the best thing of all would be to make sure as few accretas occur as possible ─ and the best way to do that is to stop doing so many non-indicated cesareans.
Risk Factors for Accreta
There are a number of risk factors for accretas; placenta previa (low-lying placenta) is the most obvious one. Most accretas occur in conjunction with a previa, although it's possible to have an accreta without a previa.
Outside of previa, a previous uterine instrumentation/surgery is probably the most important risk factor for accreta. This includes:
If the embryo does not implant too near the damaged area, placentation is usually normal. But if the embryo implants near the damaged area, then placentation is more likely to be abnormal. It all depends on the extent of the damage and exactly where the embryo implants in relation to that damage.
Maternal age is also a risk factor for accreta. Older moms (over 35) are at higher risk for abnormal attachment of the placenta, probably because subtle damage to the uterine lining can occur over the years.
Prior fertility procedures and an IVF pregnancy seem to also be associated with accreta. Again, damage to the uterine lining is thought to be the issue.
Of all the risk factors for accreta, a high underlying cesarean rate is the most preventable one.
Symptoms of Accreta
If you're pregnant and have risk factors for accreta, how would you know if you had one?
The most consistent symptom of a possible accreta is vaginal bleeding in the second trimester and beyond.
If you've had vaginal spotting in the first trimester, don't panic. This is not unusual and many viable pregnancies experience it. If it's persistent, copious, or painful, you should have it checked out to rule out problems like ectopic pregnancy, but most cases are unremarkable.
If, however, the bleeding persists into the second trimester, that may be a sign of a more serious problem, such as placental abruption (placenta detaching prematurely) or placenta previa (low-lying placenta), which can be significant complications of their own. At times it's associated with placenta accreta, either in conjunction with a previa or independent of one.
Painless bleeding is often characteristic of placenta previa, but some sources report that painful bleeding or a persistent aching may be more characteristic of previa-accretas.
However, a lack of bleeding or lack of pain does not guarantee an absence of accreta. Sometimes there is no warning that an accreta is present until the woman gives birth, the placenta doesn't come, and the woman starts hemorrhaging. This is why many care providers want a routine ultrasound to check placental placement in women with a prior cesarean.
Sometimes prenatal testing will show a raised AFP (alphafetoprotein) level in a woman with an accreta. Presence of blood in the urine can also suggest a percreta that has intruded into the woman's bladder.
Occasionally an accreta causes a uterine rupture (which can happen as early as the first trimester), so strong abdominal pain is another alarming symptom which deserves prompt medical investigation. Some people speculate that many uterine ruptures in VBACs may actually be related more to an abnormally-attached placenta than a true weakness in the scar.
Bottom line, the most common symptom is vaginal bleeding after the first trimester. This is a symptom that should always be evaluated, and especially so in a woman with a prior cesarean. A detailed ultrasound can be performed which will help determine the cause of the bleeding.
Incidence of Accreta
The actual numerical incidence of placenta accreta in the overall population is usually quoted as about 1 in 2,500 pregnancies (or about 0.04%), based on a study from the mid-1990s. However, a recent study from the U.K. found a somewhat lower incidence of accreta of about 0.017%:
However, there is no denying that the overall incidence of accreta has increased over the years. One recent study found:
Although accretas can occur without a prior cesarean, most cases these days involve a previous cesarean scar. Studies have found that about 60-80% of all accretas occur in women with at least one prior cesarean. Although accreta is an overall rare complication, it is one of the most serious "downstream" risks associated with cesareans.
Although there are many accreta risk factors that have increased over the years (higher maternal age at childbirth, more infertility procedures and IVF pregnancies, increase in uterine procedures like D&Cs, myomectomies, etc.), it's clear that the huge increase in cesarean rates has been the most important factor in the rise of accreta.
It's also clear from the research that the risk for placenta accreta rises strongly with each successive cesarean. However, the exact numerical risk varies from study to study, and may be impacted by other factors like age, parity, etc.
In one early study (Clark 1985), the absolute risks for accreta (with or without previa) were:
Research is clear that when a low-lying placenta is present in a woman with prior cesareans, there should be a strong index of suspicion for placenta accreta.
Of course, it's important not to panic. Not all women with a low-lying placenta and a history of cesareans develop accreta. Many low-lying placentas early in pregnancy "migrate" higher by term.
On the other hand, the more cesareans, the less likely it is to "migrate." So while there is no need to panic over a low anterior placenta early in pregnancy, even when you have had prior cesareans, follow-up is definitely prudent.
[My story: I had a low anterior placenta early in my 3rd pregnancy, along with a history of 2 prior cesareans, a situation which is a bit ominous. Yet my placenta "migrated" just fine, and thankfully I had no issues with previa or accreta at all.]
Obstetric care providers walk a difficult line in knowing how aggressive to be about testing in pregnancies after cesareans in order to look for problems like previa and accreta. Early testing may alert them to a problem sooner than later, yet may also cause unneeded alarm due to false positives.
Because of the potential for serious complications with accreta, most providers strongly favor at least one ultrasound in the second or third trimester to check placental placement in women with a prior cesarean. Women with bleeding, pain, or tenderness should receive early, more aggressive assessment as their symptoms dictate.
Of course, the final decision about prenatal testing always remains with the mother, but because some accretas are asymptomatic until delivery, most care providers feel that at least one ultrasound assessment at some point is prudent in women with a history of cesarean or other uterine instrumentation.
Summary
Placenta accreta is a very serious complication of pregnancy after cesarean. Bleeding after the first trimester is the most important symptom and should always be evaluated.
Although there are a number of risk factors for accreta, a prior cesarean is the most important. The risk is highest in women with multiple repeat cesareans, but accreta (and even percreta) sometimes occurs even after only one cesarean.
This is why it's so important that non-indicated cesareans be avoided whenever possible.
*Next up: Risks associated with placenta accreta, treatment choices, and a cautionary story
Research References
Increase in Incidence of Abnormal Placentation
Obstet Gynecol Clin North Am. 2013 Mar;40(1):137-54. doi: 10.1016/j.ogc.2012.12.002. Placenta accreta, increta, and percreta. Wortman AC, Alexander JM. PMID: 23466142
Am J Obstet Gynecol. 2005 May;192(5):1458-61. Abnormal placentation: twenty-year analysis. Wu S, Kocherginsky M, Hibbard JU. PMID: 15902137
As mentioned in Part One of this series, placenta accreta is an abnormally attached placenta. However, the severity can vary, leading to three different types of "morbidly adherent" placentas.
To review, each month the lining of a woman's uterus (the endometrium) changes in anticipation of a possible pregnancy, becoming the decidua if pregnancy occurs. Among other functions, the decidua helps keep the placenta from invading the mother's uterus.
In placenta accreta, the decidua is thin or deficient, allowing the placenta to attach itself directly into the maternal tissues. How deeply it attaches determines the severity of the accreta.
 |
| Konijeti 2009, Rev Urol |
In the most severe form, Placenta Percreta, the placenta grows not only into the muscle of the uterus but through the outer layer (serosa) and often into adjacent structures nearby. This is an extremely life-threatening complication because percretas usually grow into the mother's bladder or bowels, the uterus may rupture, and women can suffer severe injuries or even die from it.
Thankfully, most accretas don't involve an increta or a percreta. But even on its own, accreta is a serious complication.
Fortunately, foreknowledge of an accreta, careful management protocols, and being in the right delivery setting can significantly lower the risk for mortality and morbidity. But the best thing of all would be to make sure as few accretas occur as possible ─ and the best way to do that is to stop doing so many non-indicated cesareans.
Risk Factors for Accreta
There are a number of risk factors for accretas; placenta previa (low-lying placenta) is the most obvious one. Most accretas occur in conjunction with a previa, although it's possible to have an accreta without a previa.
Outside of previa, a previous uterine instrumentation/surgery is probably the most important risk factor for accreta. This includes:
- Cesareans
- D&C (Dilation and Curettage, whether for miscarriage, abortion, menstrual problems, or retained placental fragments)
- Myomectomies (fibroid removals)
- Embolizations (for fibroid removals)
- Uterine ablations
- Possibly various fertility procedures, especially hysteroscopic surgeries
If the embryo does not implant too near the damaged area, placentation is usually normal. But if the embryo implants near the damaged area, then placentation is more likely to be abnormal. It all depends on the extent of the damage and exactly where the embryo implants in relation to that damage.
Maternal age is also a risk factor for accreta. Older moms (over 35) are at higher risk for abnormal attachment of the placenta, probably because subtle damage to the uterine lining can occur over the years.
Prior fertility procedures and an IVF pregnancy seem to also be associated with accreta. Again, damage to the uterine lining is thought to be the issue.
Of all the risk factors for accreta, a high underlying cesarean rate is the most preventable one.
Symptoms of Accreta
If you're pregnant and have risk factors for accreta, how would you know if you had one?
The most consistent symptom of a possible accreta is vaginal bleeding in the second trimester and beyond.
If you've had vaginal spotting in the first trimester, don't panic. This is not unusual and many viable pregnancies experience it. If it's persistent, copious, or painful, you should have it checked out to rule out problems like ectopic pregnancy, but most cases are unremarkable.
If, however, the bleeding persists into the second trimester, that may be a sign of a more serious problem, such as placental abruption (placenta detaching prematurely) or placenta previa (low-lying placenta), which can be significant complications of their own. At times it's associated with placenta accreta, either in conjunction with a previa or independent of one.
Painless bleeding is often characteristic of placenta previa, but some sources report that painful bleeding or a persistent aching may be more characteristic of previa-accretas.
However, a lack of bleeding or lack of pain does not guarantee an absence of accreta. Sometimes there is no warning that an accreta is present until the woman gives birth, the placenta doesn't come, and the woman starts hemorrhaging. This is why many care providers want a routine ultrasound to check placental placement in women with a prior cesarean.
Sometimes prenatal testing will show a raised AFP (alphafetoprotein) level in a woman with an accreta. Presence of blood in the urine can also suggest a percreta that has intruded into the woman's bladder.
Occasionally an accreta causes a uterine rupture (which can happen as early as the first trimester), so strong abdominal pain is another alarming symptom which deserves prompt medical investigation. Some people speculate that many uterine ruptures in VBACs may actually be related more to an abnormally-attached placenta than a true weakness in the scar.
Bottom line, the most common symptom is vaginal bleeding after the first trimester. This is a symptom that should always be evaluated, and especially so in a woman with a prior cesarean. A detailed ultrasound can be performed which will help determine the cause of the bleeding.
Incidence of Accreta
The actual numerical incidence of placenta accreta in the overall population is usually quoted as about 1 in 2,500 pregnancies (or about 0.04%), based on a study from the mid-1990s. However, a recent study from the U.K. found a somewhat lower incidence of accreta of about 0.017%:
The estimated incidence of placenta accreta/increta/percreta was 1.7 per 10,000 maternities overall; 577 per 10,000 in women with both a previous caesarean delivery and placenta praevia.The incidence of accreta can vary quite a bit between studies. Areas which have a high underlying rate of cesareans, studies with older or more parous moms, and studies done in large regional hospitals (where complicated cases get referred) will have higher accreta rates than a study of the overall population of a country. Therefore, an exact incidence of accreta is hard to pinpoint.
However, there is no denying that the overall incidence of accreta has increased over the years. One recent study found:
The incidence of placenta accreta has increased 13-fold since the early 1900s and directly correlates with the increasing cesarean delivery rate.Association with Prior Cesarean
Although accretas can occur without a prior cesarean, most cases these days involve a previous cesarean scar. Studies have found that about 60-80% of all accretas occur in women with at least one prior cesarean. Although accreta is an overall rare complication, it is one of the most serious "downstream" risks associated with cesareans.
Although there are many accreta risk factors that have increased over the years (higher maternal age at childbirth, more infertility procedures and IVF pregnancies, increase in uterine procedures like D&Cs, myomectomies, etc.), it's clear that the huge increase in cesarean rates has been the most important factor in the rise of accreta.
It's also clear from the research that the risk for placenta accreta rises strongly with each successive cesarean. However, the exact numerical risk varies from study to study, and may be impacted by other factors like age, parity, etc.
In one early study (Clark 1985), the absolute risks for accreta (with or without previa) were:
- 0.01% accreta (unscarred uterus)
- 0.16% accreta after one prior cesarean (undergoing second cesarean)
- 0.82% accreta after two prior cesareans (undergoing third cesarean)
- 1.1% accreta after three prior cesareans (undergoing fourth cesarean)
- 6.9% accreta after four or more prior cesareans (undergoing fifth or more cesarean)
- 0.002% (unscarred uterus)
- 0.1% after one prior cesarean
- 0.3% after two or more prior cesareans
- 0.24% of women undergoing their first cesarean (previously unscarred)
- 0.31% of women undergoing their second cesarean (one prior cesarean)
- 0.57% of women undergoing their third cesarean (two prior cesareans)
- 2.13% of women undergoing their fourth cesarean (three prior cesareans)
- 2.33% of women undergoing their fifth cesarean (four prior cesareans)
- 6.74% of women undergoing their sixth or more cesarean (five or more prior cesareans)
Obviously, multiple prior cesareans is a very important risk factor for accretas.
On the other hand, it's also important to point out that most women who are having higher-order cesareans will not experience accreta. However, it is such an alarming and life-threatening condition that even these relatively small incidences carry a huge burden of complications, cost, and potential loss of life.
This is why accreta is such a big deal, and why it is so important NOT to do routine repeat cesareans, particularly in women who want large families.
In a woman with a cesarean history and current placenta previa, multiple prior cesareans increases the likelihood that the previa will be complicated by accreta. In the Silver 2006 study, of those women who already had previa, the risk for accreta was strongly associated with the number of prior cesareans:
On the other hand, it's also important to point out that most women who are having higher-order cesareans will not experience accreta. However, it is such an alarming and life-threatening condition that even these relatively small incidences carry a huge burden of complications, cost, and potential loss of life.
This is why accreta is such a big deal, and why it is so important NOT to do routine repeat cesareans, particularly in women who want large families.
In a woman with a cesarean history and current placenta previa, multiple prior cesareans increases the likelihood that the previa will be complicated by accreta. In the Silver 2006 study, of those women who already had previa, the risk for accreta was strongly associated with the number of prior cesareans:
- 3% of women with previa having their first cesarean also had accreta
- 11% of women with previa having their second cesarean also had accreta
- 40% of women with previa having their third cesarean also had accreta
- 61% of women with previa having their fourth cesarean also had accreta
- 67% of women with previa having their fifth or more cesarean also had accreta
Of course, it's important not to panic. Not all women with a low-lying placenta and a history of cesareans develop accreta. Many low-lying placentas early in pregnancy "migrate" higher by term.
On the other hand, the more cesareans, the less likely it is to "migrate." So while there is no need to panic over a low anterior placenta early in pregnancy, even when you have had prior cesareans, follow-up is definitely prudent.
[My story: I had a low anterior placenta early in my 3rd pregnancy, along with a history of 2 prior cesareans, a situation which is a bit ominous. Yet my placenta "migrated" just fine, and thankfully I had no issues with previa or accreta at all.]
Obstetric care providers walk a difficult line in knowing how aggressive to be about testing in pregnancies after cesareans in order to look for problems like previa and accreta. Early testing may alert them to a problem sooner than later, yet may also cause unneeded alarm due to false positives.
Because of the potential for serious complications with accreta, most providers strongly favor at least one ultrasound in the second or third trimester to check placental placement in women with a prior cesarean. Women with bleeding, pain, or tenderness should receive early, more aggressive assessment as their symptoms dictate.
Of course, the final decision about prenatal testing always remains with the mother, but because some accretas are asymptomatic until delivery, most care providers feel that at least one ultrasound assessment at some point is prudent in women with a history of cesarean or other uterine instrumentation.
Summary
Placenta accreta is a very serious complication of pregnancy after cesarean. Bleeding after the first trimester is the most important symptom and should always be evaluated.
Although there are a number of risk factors for accreta, a prior cesarean is the most important. The risk is highest in women with multiple repeat cesareans, but accreta (and even percreta) sometimes occurs even after only one cesarean.
This is why it's so important that non-indicated cesareans be avoided whenever possible.
*Next up: Risks associated with placenta accreta, treatment choices, and a cautionary story
Research References
Accreta Information
- ACOG's Committee Opinion on Management of Placenta Accreta
- RCOG's Guideline on Management of Placenta Accreta
- Wikipedia entry on Placenta Accreta
- http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0052893
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3516467/pdf/ijwh-4-587.pdf
- http://www.obgmanagement.com/fileadmin/obg_archive/pdf/1408/1408OBGM_Article2.pdf
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2777065/
- http://www.mountsinai.on.ca/care/placenta-clinic/complications/invasiveplacenta
- http://vbacfacts.com/2009/08/03/risk-of-serious-complications-increase-with-each-cesarean-surgery/
Obstet Gynecol Clin North Am. 2013 Mar;40(1):137-54. doi: 10.1016/j.ogc.2012.12.002. Placenta accreta, increta, and percreta. Wortman AC, Alexander JM. PMID: 23466142
Placenta accreta is an abnormal adherence of the placenta to the uterine wall that can lead to significant maternal morbidity and mortality. The incidence of placenta accreta has increased 13-fold since the early 1900s and directly correlates with the increasing cesarean delivery rate. The prenatal diagnosis of placenta accreta by ultrasound along with risk factors including placenta previa and prior cesarean delivery can aid in delivery planning and improved outcomes. Referral to a tertiary care center and the use of a multidisciplinary care team is recommended.Aust N Z J Obstet Gynaecol. 2004 Jun;44(3):210-3. Is placenta accreta catching up with us? Armstrong CA, Harding S, Matthews T, Dickinson JE. PMID: 15191444
...METHODS: A retrospective review of all cases of placenta accreta and variants during the period of 1998-2002...RESULTS: ...Seventy-eight percent of cases had had at least one prior Caesarean birth, and 88% of cases were associated with placenta praevia. Pre-delivery ultrasonography was performed in all cases, providing diagnostic sensitivity of 63% and specificity of 43% with a predictive value of 76%. Hysterectomy was performed in 91% of cases with median intraoperative blood loss of 3000 mL. There were no maternal deaths in the current series. CONCLUSION: A strong association between placenta accreta, placenta praevia and prior Caesarean birth has been demonstrated...Am J Obstet Gynecol. 1997 Jul;177(1):210-4. Clinical risk factors for placenta previa-placenta accreta. Miller DA, Chollet JA, Goodwin TM. PMID: 9240608
STUDY DESIGN: Hospital records were reviewed of all cases of placenta accreta confirmed histologically between January 1985 and December 1994. Additionally, we reviewed the records of all women with placenta previa and all those undergoing cesarean hysterectomy during the same period. Multiple logistic regression analysis was used to identify independent clinical risk factors for placenta accreta.... CONCLUSION: Placenta accreta occurs in approximately 1 of 2500 deliveries.Risk Factors for Abnormal Placentation
Am J Obstet Gynecol. 2005 May;192(5):1458-61. Abnormal placentation: twenty-year analysis. Wu S, Kocherginsky M, Hibbard JU. PMID: 15902137
OBJECTIVE: This study was undertaken to determine whether the rate of abnormal placentation is increasing in conjunction with the cesarean rate and to evaluate incidence, risk factors, and outcomes...RESULTS: There were 64,359 deliveries, with cesarean rates increasing from 12.5% (1982) to 23.5% (2002). The overall incidence of placenta accreta was 1 in 533. Significant risk factors for placenta accreta in our final analysis included advancing maternal age (odds ratio [OR] 1.13, 95% CI 1.089-1.194, P < .0001), 2 or more cesarean deliveries (OR 8.6, 95% CI 3.536-21.078, P < .0001), and previa (OR 51.4, 95% CI: 10.646-248.390, P < .0001). CONCLUSION: The rate of placenta accreta increased in conjunction with cesarean deliveries; the most important risk factors were previous cesarean delivery, previa, and advanced maternal age.PLoS One. 2012;7(12):e52893. doi: 10.1371/journal.pone.0052893. Epub 2012 Dec 27. Incidence and risk factors for placenta accreta/increta/percreta in the UK: a national case-control study. Fitzpatrick KE, Sellers S, Spark P, Kurinczuk JJ, Brocklehurst P, Knight M. PMID: 23300807
...METHODS: A national case-control study using the UK Obstetric Surveillance System was undertaken, including 134 women diagnosed with placenta accreta/increta/percreta between May 2010 and April 2011 and 256 control women. RESULTS: The estimated incidence of placenta accreta/increta/percreta was 1.7 per 10,000 maternities overall; 577 per 10,000 in women with both a previous caesarean delivery and placenta praevia. Women who had a previous caesarean delivery (adjusted odds ratio (aOR) 14.41, 95%CI 5.63-36.85), other previous uterine surgery (aOR 3.40, 95%CI 1.30-8.91), an IVF pregnancy (aOR 32.13, 95%CI 2.03-509.23) and placenta praevia diagnosed antepartum (aOR 65.02, 95%CI 16.58-254.96) had raised odds of having placenta accreta/increta/percreta. There was also a raised odds of placenta accreta/increta/percreta associated with older maternal age in women without a previous caesarean delivery (aOR 1.30, 95%CI 1.13-1.50 for every one year increase in age). CONCLUSIONS: Women with both a prior caesarean delivery and placenta praevia have a high incidence of placenta accreta/increta/percreta. There is a need to maintain a high index of suspicion of abnormal placental invasion in such women and preparations for delivery should be made accordingly.Acta Obstet Gynecol Scand. 2013 Apr;92(4):457-60. doi: 10.1111/aogs.12080. Placenta accreta: incidence and risk factors in an area with a particularly high rate of cesarean section. Morlando M, Sarno L, Napolitano R, Capone A, Tessitore G, Maruotti GM, Martinelli P. PMID: 23347183
...The aim of this study was to investigate the change in the incidence of placenta accreta and associated risk factors along four decades, from the 1970s to 2000s, in a tertiary south Italian center. We analyzed all cases of placenta accreta in a sample triennium for each decade. The incidence increased from 0.12% during the 1970s, to 0.31% during the 2000s. During the same period, cesarean section rates increased from 17 to 64%. Prior cesarean section was the only risk factor showing a significant concomitant rise. Our results reinforce cesarean section as the most significant predisposing condition for placenta accreta.Placenta. 2012 Apr;33(4):244-51. doi: 10.1016/j.placenta.2011.11.010. Epub 2012 Jan 28. Placenta accreta: pathogenesis of a 20th century iatrogenic uterine disease. Jauniaux E, Jurkovic D. PMID: 22284667
Placenta accreta refers to different grades of abnormal placental attachment to the uterine wall, which are characterised by invasion of trophoblast into the myometrium. Placenta accreta has only been described and studied by pathologists for less than a century. The fact that the first detailed description of a placenta accreta happened within a couple of decades of major changes in the caesarean surgical techniques is highly suggestive of a direct relationship between prior uterine surgery and abnormal placenta adherence. Several concepts have been proposed to explain the abnormal placentation in placenta accreta including a primary defect of the trophoblast function, a secondary basalis defect due to a failure of normal decidualization and more recently an abnormal vascularisation and tissue oxygenation of the scar area. The vast majority of placenta accreta are found in women presenting with a previous history of caesarean section and a placenta praevia. Recent epidemiological studies have also found that the strongest risk factor for placenta praevia is a prior caesarean section suggesting that a failure of decidualization in the area of a previous uterine scar can have an impact on both implantation and placentation. Ultrasound studies of uterine caesarean section scar have shown that large and deep myometrial defects are often associated with absence of re-epithelialisation of the scar area. These findings support the concept of a primary deciduo-myometrium defect in placenta accreta, exposing the myometrium and its vasculature below the junctional zone to the migrating trophoblast. The loss of this normal plane of cleavage and the excessive vascular remodelling of the radial and arcuate arteries can explain the in-vivo findings and the clinical consequence of placenta accreta. Overall these data support the concept that abnormal decidualization and trophoblastic changes of the placental bed in placenta accreta are secondary to the uterine scar and thus entirely iatrogenic.
Placenta Accreta and Prior Cesareans
Obstet Gynecol. 2006 Jun;107(6):1226-32. Maternal morbidity associated with multiple repeat cesarean deliveries. Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, Moawad AH, Caritis SN, Harper M, Wapner RJ, Sorokin Y, Miodovnik M, Carpenter M, Peaceman AM, O'Sullivan MJ, Sibai B, Langer O, Thorp JM, Ramin SM, Mercer BM; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. PMID: 16738145
Obstet Gynecol. 2006 Jun;107(6):1226-32. Maternal morbidity associated with multiple repeat cesarean deliveries. Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, Moawad AH, Caritis SN, Harper M, Wapner RJ, Sorokin Y, Miodovnik M, Carpenter M, Peaceman AM, O'Sullivan MJ, Sibai B, Langer O, Thorp JM, Ramin SM, Mercer BM; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. PMID: 16738145
...METHODS: Prospective observational cohort of 30,132 women who had cesarean delivery without labor in 19 academic centers over 4 years (1999-2002). RESULTS:...The risks of placenta accreta, cystotomy, bowel injury, ureteral injury, and ileus, the need for postoperative ventilation, intensive care unit admission, hysterectomy, and blood transfusion requiring 4 or more units, and the duration of operative time and hospital stay significantly increased with increasing number of cesarean deliveries. Placenta accreta was present in 15 (0.24%), 49 (0.31%), 36 (0.57%), 31 (2.13%), 6 (2.33%), and 6 (6.74%) women undergoing their first, second, third, fourth, fifth, and sixth or more cesarean deliveries, respectively. Hysterectomy was required in 40 (0.65%) first, 67 (0.42%) second, 57 (0.90%) third, 35 (2.41%) fourth, 9 (3.49%) fifth, and 8 (8.99%) sixth or more cesarean deliveries. In the 723 women with previa, the risk for placenta accreta was 3%, 11%, 40%, 61%, and 67% for first, second, third, fourth, and fifth or more repeat cesarean deliveries, respectively. CONCLUSION: Because serious maternal morbidity increases progressively with increasing number of cesarean deliveries, the number of intended pregnancies should be considered during counseling regarding elective repeat cesarean operation versus a trial of labor and when debating the merits of elective primary cesarean delivery.Obstet Gynecol. 1985 Jul;66(1):89-92. Placenta previa/accreta and prior cesarean section. Clark SL, Koonings PP, Phelan JP. PMID: 4011075
To assess the relationship between increasing numbers of previous cesarean sections and the subsequent development of placenta previa and placenta accreta, the records of all patients presenting to labor and delivery with the diagnosis of placenta previa between 1977 and 1983 were examined. Of a total of 97,799 patients, 292 (0.3%) had a placenta previa. The risk of placenta previa was 0.26% with an unscarred uterus and increased almost linearly with the number of prior cesarean sections to 10% in patients with four or more. The effect of advancing age and parity on the incidence of placenta previa was much less dramatic. Patients presenting with a placenta previa and an unscarred uterus had a 5% risk of clinical placenta accreta. With a placenta previa and one previous cesarean section, the risk of placenta accreta was 24%; this risk continued to increase to 67% (two of three) with a placenta previa and four or more cesarean sections. Possible mechanisms and clinical implications are discussed.Am J Obstet Gynecol. 1997 Jul;177(1):210-4. Clinical risk factors for placenta previa-placenta accreta. Miller DA, Chollet JA, Goodwin TM. PMID: 9240608
OBJECTIVE: Our purpose was to define the clinical risk factors associated with placenta previa-placenta accreta. STUDY DESIGN: Hospital records were reviewed of all cases of placenta accreta confirmed histologically between January 1985 and December 1994. Additionally, we reviewed the records of all women with placenta previa and all those undergoing cesarean hysterectomy during the same period. Multiple logistic regression analysis was used to identify independent clinical risk factors for placenta accreta. RESULTS: Among 155,670 deliveries, 62 (1/2510) were complicated by histologically confirmed placenta accreta. Placenta accreta occurred in 55 of 590 (9.3%) women with placenta previa and in 7 of 155,080 (1/22,154) without placenta previa (relative risk 2065, 95% confidence interval 944 to 4516, p < 0.0001). Among women with placenta previa, advanced maternal age (> or = 35 years) and previous cesarean delivery were independent risk factors for placenta accreta. Placenta accreta was present in 36 of 124 (29%) cases in which the placenta was implanted over the uterine scar and in 4 of 62 (6.5%) cases in which it was not (relative risk 4.5, 95% confidence interval 1.68 to 12.07). Among women with placenta previa, the risk of placenta accreta ranged from 2% in women < 35 years old with no previous cesarean deliveries to almost 39% in women with two or more previous cesarean deliveries and an anterior or central placenta previa. CONCLUSION: Placenta accreta occurs in approximately 1 of 2500 deliveries. Among women with placenta previa, the incidence is nearly 10%. In this high-risk group advanced maternal age and previous cesarean section are independent risk factors.Int J Gynaecol Obstet. 1995 Oct;51(1):25-31. Placenta previa and previous cesarean section. To WW, Leung WC. PMID: 8582514
OBJECTIVE: To assess the relationship between previous cesarean section and subsequent development of placenta previa and placenta previa with accreta. METHOD: The records of all patients delivered with the diagnosis of placenta previa during the 10-year period from 1984 to 1993 were reviewed. RESULTS: From a total of 50,485 deliveries, 421 (0.83%) had placenta previa, 43 (10.2%) of whom had a history of previous cesarean section. The incidence of placenta previa was significantly increased in those with a previous cesarean section (1.31%) compared with those with an unscarred uterus (0.75%) (R.R. 1.64). This risk increased as the number of previous cesarean sections increased (R.R. 1.53 for one previous section, 2.63 for two or more). The incidence of an anterior placenta previa and placenta accreta was significantly increased in those with previous cesarean scars. The incidence of placenta accreta was 1.18% among patients with placenta previa, 80% being in patients with previous cesarean section. The relative risk for placenta accreta in patients with placenta previa was 35 times higher in those with a previous cesarean section than in those with an unscarred uterus. CONCLUSION: The association of previous cesarean section with placenta previa and placenta previa accreta is confirmed. Patients with an antepartum diagnosis of placenta previa who have had a previous cesarean section should be considered at high risk for developing placenta accreta.Semin Perinatol. 2012 Oct;36(5):315-23. doi: 10.1053/j.semperi.2012.04.013. Implications of the first cesarean: perinatal and future reproductive health and subsequent cesareans, placentation issues, uterine rupture risk, morbidity, and mortality. Silver RM. PMID: 23009962
Rates of cesarean delivery have substantially increased worldwide during the past 30 years. Indeed, almost one-third of deliveries in the United States are cesareans. Most cesareans are safe, and major complications are uncommon. However, there is a "concealed" downside to cesarean deliveries. There are rare but life-threatening morbidities that may occur, which are often overlooked because most cesareans go well. In addition, subsequent pregnancies are fraught with an increased risk of both maternal and fetal complications. The worst of these are associated with placental problems such as previa, abruption, and accreta. The risk dramatically worsens in patients with multiple repeat cesarean deliveries. This article will summarize and highlight the implications of the rising cesarean rate on maternal and fetal morbidity and mortality.
No comments:
Post a Comment